Overview
Ebstein anomaly is a rare heart condition that's present at birth. That means it's a congenital heart defect.
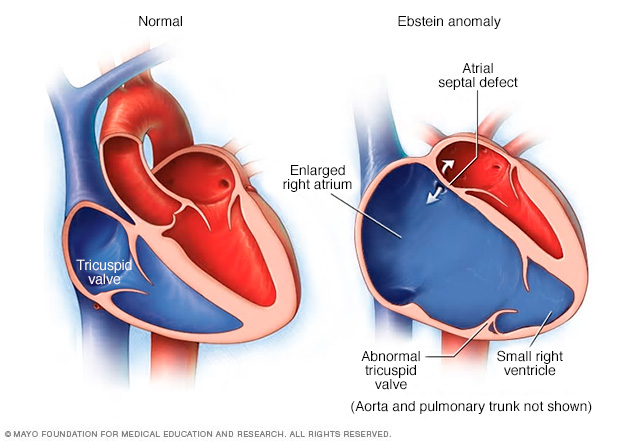
In this condition, the valve that separates the top and bottom right heart chambers does not form correctly. This valve is called the tricuspid valve. As a result, the valve does not close as it should. Blood moves backward from the bottom to top chamber, making it harder for the heart to work.
In people with Ebstein anomaly, the heart can grow larger. The condition can lead to heart failure.
Treatment of Ebstein anomaly depends on the symptoms. Some people without symptoms only need regular health checkups. Others may need medicines and surgery.
Symptoms
Some babies born with Ebstein anomaly have few or no symptoms. Others have a tricuspid valve that leaks severely and causes more-noticeable symptoms. Sometimes symptoms don't occur until later in life.
Symptoms of Ebstein anomaly may include:
- Blue or gray lips or fingernails. Depending on skin color, these color changes may be harder or easier to see.
- Fatigue.
- Feeling of a pounding or rapid heartbeat or irregular heartbeats.
- Shortness of breath, especially with activity.
When to see a doctor
Serious heart conditions in a baby are often diagnosed at birth or during pregnancy.
Make a health appointment if you or your baby has symptoms of a possible heart condition. These symptoms include feeling short of breath or easily tired with little activity, irregular heartbeats, or changes in skin color. You may be sent to a doctor trained in heart diseases, called a cardiologist.
Causes
Ebstein anomaly is a heart condition that a person is born with. The cause is not known. To understand more about Ebstein anomaly, it may help to know how the heart works.
How the heart works
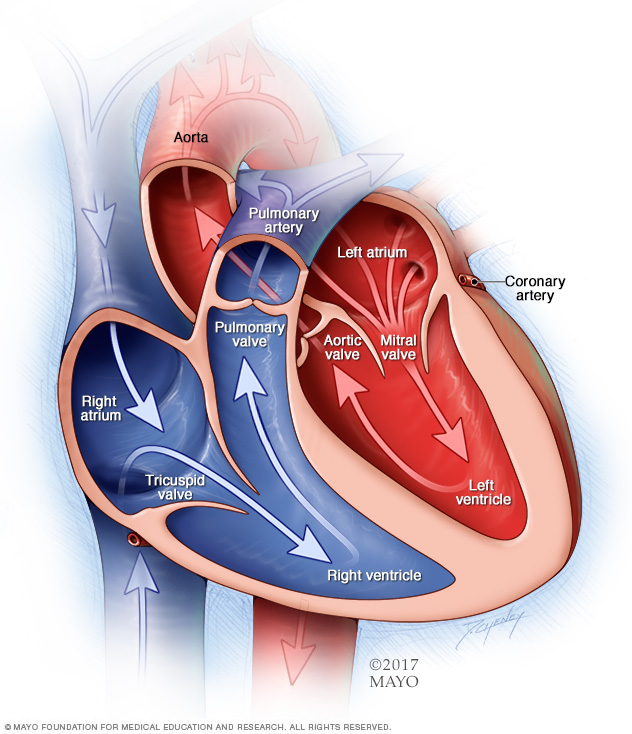
The typical heart has four chambers.
- The two upper chambers are called the atria. They receive blood.
- The two lower chambers are called the ventricles. They pump blood.
Four valves open and close to let blood flow in one direction through the heart. Each valve has two or three strong, thin flaps of tissue. The flaps are called leaflets or cusps.
- A valve that is closed stops blood from flowing into the next chamber.
- A closed valve also prevents blood from going back to the previous chamber.
In a typical heart, the tricuspid valve sits between the two right heart chambers. In Ebstein anomaly, the tricuspid valve is lower than usual in the right lower heart chamber. Also, the shape of the tricuspid valve's flaps is changed. This can cause blood to flow backward into the right upper heart chamber. When this happens, the condition is called tricuspid valve regurgitation.
Heart conditions associated with Ebstein anomaly
Babies born with Ebstein anomaly may have other heart conditions, including:
- Holes in the heart. A hole in the heart can lower the amount of oxygen in the blood. Many babies with Ebstein anomaly have a hole between the two upper chambers of the heart. This hole is called an atrial septal defect. Or there may be an opening called a patent foramen ovale, also called a PFO. A PFO is a hole between the upper heart chambers that all babies have before birth. It usually closes after birth. But it can stay open in some people.
- Irregular heartbeats, called arrhythmias. An irregular heartbeat can include a fluttering, pounding or racing heartbeat. Changes in the heartbeat can make it harder for the heart to work as it should.
- Wolff-Parkinson-White (WPW) syndrome. In this condition, an extra signaling pathway between the heart's upper and lower chambers causes a fast heartbeat and fainting.
Risk factors
Ebstein anomaly occurs as the baby, also called a fetus, grows in the womb during pregnancy.
Researchers aren't sure exactly what increases the risk of Ebstein anomaly. Genetics and environmental factors are believed to be involved. Using some medicines during pregnancy, such as lithium, might increase the risk of Ebstein anomaly in the baby.
Complications
Possible complications of Ebstein anomaly include:
- Irregular heartbeats.
- Heart failure.
- Sudden cardiac arrest.
- Stroke.
Pregnancy and Ebstein anomaly
It may be possible to have a successful pregnancy with mild Ebstein anomaly. But pregnancy, labor and delivery put extra strain on the heart. Rarely, extreme complications can develop that can cause serious health concerns in the mother or baby.
Before becoming pregnant, talk with your healthcare team about the possible risks and complications. Together you can plan for any special care needed during pregnancy.
Diagnosis
To diagnose Ebstein anomaly, a healthcare professional examines the baby and listens to the heart and lungs. A heart sound called a murmur may be heard.
Tests
Tests that are done to help diagnose Ebstein anomaly include:
- Pulse oximetry. In this test, a sensor attached to a finger or toe measures the amount of oxygen in the blood.
- Echocardiogram. Sound waves are used to create pictures of the beating heart. An echocardiogram can show how blood flows through the heart and heart valves.
- Electrocardiogram (ECG or EKG). This simple test checks the heartbeat. Sticky patches attach to the chest and sometimes the arms and legs. Wires connect the patches to a computer, which prints or displays the results.
- Holter monitor. This portable ECG device is worn for a day or more to record the heart's activity during daily activities.
- Chest X-ray. A chest X-ray is a picture of the heart, lungs and blood vessels. It can show if the heart is enlarged.
- Cardiac MRI. A cardiac MRI uses magnetic fields and radio waves to create images of the heart. This test can give a detailed view of the tricuspid valve. It also shows the size of the heart chambers and how well they work.
- Exercise stress tests. These tests often involve walking on a treadmill or riding a stationary bike while the heart is checked. An exercise stress test can show how the heart reacts to exercise.
- Electrophysiology study (EP study). A doctor threads a thin, flexible tube called a catheter into a blood vessel and guides it to the heart. More than one catheter may be used. Sensors on the tip of the catheter give off electrical signals and record the heart's electricity. This test helps show which part of the heart is causing a fast or irregular heartbeat. Treatment of an irregular heartbeat may be done during this test.
- Cardiac catheterization. A doctor places a long, thin flexible tube into a blood vessel, usually in the groin or wrist. It's guided to the heart. Dye flows through the tube to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video. During the test, pressures and oxygen levels can be measured in different parts of the heart. Some heart disease treatments also can be done during this test.
Treatment
Treatment of Ebstein anomaly depends on:
- How severe the condition is.
- The symptoms.
The goals of treatment are to:
- Reduce symptoms.
- Prevent complications, such as irregular heartbeats and heart failure.
Treatment may include regular health checkups, medicines, or a heart procedure or surgery.
Regular health checkups
If Ebstein anomaly isn't causing irregular heartbeats or other symptoms, regular health checkups may be all that's needed.
Checkups are usually done at least once a year. The checkup usually includes a physical exam and imaging tests to look at the heart.
Medications
If you have Ebstein anomaly, you may get medicine to:
- Control irregular heartbeats or other changes in the heartbeat.
- Prevent fluid buildup in the body. Too much fluid in the body can be a sign of heart failure.
- Prevent blood clots. Blood clots may happen if the condition also occurs with a hole in the heart.
Some babies also are given an inhaled substance called nitric oxide to help improve blood flow to the lungs.
Surgery or other procedures
Surgery is typically done if Ebstein anomaly causes severe tricuspid regurgitation and there is heart failure or increasing difficulty with exercise.
Surgery also may be recommended if other symptoms, such as some irregular heartbeats, are very bad or affecting quality of life.
If surgery is needed, it's important to choose a surgeon who's familiar with Ebstein anomaly. The surgeon should have training and experience doing procedures to fix the condition.
Surgery to treat Ebstein anomaly and related heart conditions may include:
-
Tricuspid valve repair. This open-heart surgery fixes a damaged tricuspid valve. The surgeon may patch holes or tears in the valve flaps or remove extra tissue around the valve opening. Other repairs also may be done.
A type of valve repair called the cone procedure may be done. The heart surgeon separates the heart muscle from the tissue that should have formed the tricuspid valve. The tissue is then used to create a working tricuspid valve.
Sometimes, the valve might need to be repaired again or replaced in the future.
- Tricuspid valve replacement. If the valve can't be repaired, surgery to replace the valve may be needed. Tricuspid valve replacement surgery may be done as open-heart surgery or minimally invasive surgery. The surgeon removes the damaged or diseased valve and replaces it with a valve made from cow, pig or human heart tissue. This is called a biologic valve. Mechanical valves aren't used often for tricuspid valve replacement.
- Closure of the atrial septal defect. This surgery is done to fix a hole between the upper chambers of the heart. Other heart conditions also may be repaired during this surgery.
- Maze procedure. If Ebstein anomaly causes irregular heartbeats, this treatment may be done during valve repair or replacement surgery. The surgeon makes small cuts in the upper chambers of the heart to create a pattern of scar tissue. The pattern is called a maze. The heart's signals can't pass through scar tissue. So the maze blocks the irregular heart rhythms. Heat or cold energy also can be used to create the scars.
-
Radiofrequency catheter ablation. This treatment is done to correct fast or irregular heartbeats. The doctor inserts one or more thin, flexible tubes called catheters into a blood vessel, usually in the groin. The doctor guides them to the heart.
Sensors at the tips of the catheters use heat, called radiofrequency energy, to damage a small area of heart tissue. This creates scarring, which blocks the heart signals that cause the irregular heartbeats.
- Heart transplant. If severe Ebstein anomaly is causing the heart to fail, a heart transplant might be needed.
Coping and support
These tips can help you manage Ebstein anomaly symptoms and improve comfort.
- Get regular health checkups. Choose a heart doctor trained in treating heart conditions present at birth. This type of doctor is called a congenital cardiologist. Tell your healthcare team if there are any new symptoms, or if symptoms get worse.
- Take medicines as told. Taking the right dose at the right time may help ease symptoms such as racing heartbeats, fatigue and shortness of breath.
- Stay active. Be as physically active as possible. Exercise can help strengthen the heart and improve blood flow. Ask your healthcare team how much exercise is right for you or your child. Some people who are born with a heart condition may need to limit exercise or sports activities. But many others with a congenital heart defect can participate in such activities.
- Create a helpful network. Living with a heart condition can make some people feel stressed or anxious. Talking to a therapist or counselor may be helpful.
- Join a support group. Talking with other people who've experienced the same situation may bring comfort and encouragement. Ask your healthcare team if there are any Ebstein anomaly support groups in your area.
Preparing for an appointment
You may be sent to a doctor trained in treating heart conditions, called a cardiologist. Here's some information to help you get ready for your appointment.
What you can do
When you make the appointment, ask if there's anything you need to do ahead of time. For example, you may be told not to eat or drink for a while before certain tests.
Make a list of:
- The symptoms, including any that may seem unrelated to Ebstein anomaly. Note when they started.
- Important personal information, including a family history of heart conditions.
- All medicines, vitamins or other supplements. Include the dosages.
- Questions to ask your healthcare team.
If you're seeing a new healthcare professional, get a copy of medical records. Send them to the new office.
For Ebstein anomaly, specific questions to ask the healthcare professional include:
- What's the most likely cause of these symptoms?
- What tests are needed?
- What treatments are available? Which do you recommend and why?
- What are the side effects of treatment?
- Are there any diet or activity restrictions?
- Is there any information that I can take home? What websites do you recommend?
Don't hesitate to ask other questions.
What to expect from your doctor
Your healthcare professional is likely to ask you questions, such as:
- Do the symptoms come and go, or do they happen all the time?
- How severe are the symptoms?
- Does anything improve the symptoms?
- What, if anything, makes the symptoms worse?
© 1998-2026 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use


